What is Psoriasis?
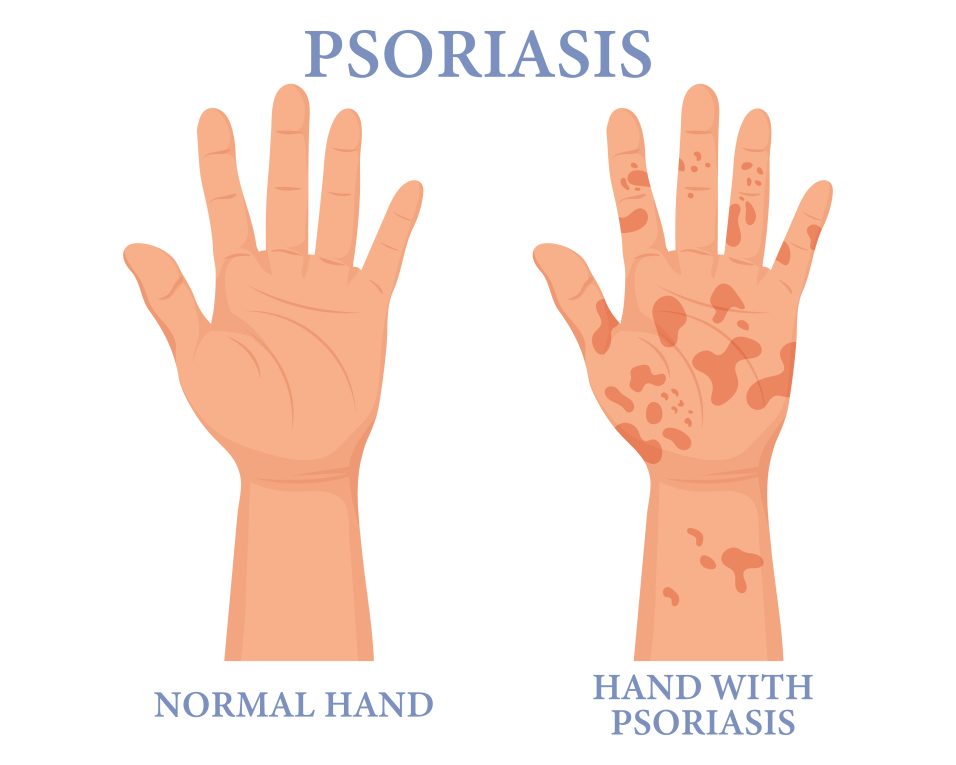
Psoriasis is a chronic inflammatory skin problem characterised by red and scaly patches due to the rapid production of new skin cells. This cells buildup forms scales and red patches that can be itchy and sometimes also painful. The common areas affected are the elbows, knees, scalp, and lower back, although psoriasis can occur anywhere on the body.
Psoriasis is a long-term condition with periods of remission and flare-ups. For some, it is a mild irritation, while for others, it can significantly impact quality of life. Despite being a skin condition, psoriasis has systemic implications, as it is associated with an increased risk of other health issues such as cardiovascular disease, arthritis, and mental health disorders.
Types of Psoriasis
- Plaque Psoriasis: This is the most common form, affecting around 80% of people with psoriasis. It causes raised, inflamed patches of skin covered with silvery-white scales. These plaques often appear on the scalp, knees, elbows, and lower back.
- Guttate Psoriasis: This form often affects children and young adults. It presents as small, dot-like lesions, usually triggered by bacterial infections like strep throat.
- Inverse Psoriasis: Characterized by smooth, red lesions that form in skin folds, such as the armpits, under the breasts, and around the groin. It tends to worsen with friction and sweating.
- Pustular Psoriasis: A rarer form, pustular psoriasis causes pus-filled blisters surrounded by red skin. It can be localized to certain areas like the hands and feet or spread across larger parts of the body.
- Erythrodermic Psoriasis: The rarest but most severe form, erythrodermic psoriasis can cover the entire body with a red, peeling rash. This condition can be life-threatening and requires quick medical attention.
Symptoms of Psoriasis
Common Psoriasis symptoms include:
- Red patches of skin covered with thick, silvery scales
- Dry, cracked skin that may bleed or itch
- Itching, burning, or soreness in the affected areas
- Thickened, pitted, or ridged nails
- Stiff and swollen joints (in cases of psoriatic arthritis)
Psoriasis often goes through cycles, with periods of remission followed by flare-ups, which can be triggered by stress, injury to the skin, certain medications and other factors.
Causes of Psoriasis
The exact cause of psoriasis remains unknown, but research suggests that it is related to an immune system problem. In psoriasis, the immune system mistakenly attacks healthy skin cells, leading to an overproduction of new skin cells. Normally, skin cells are replaced every 28 to 30 days, but in psoriasis, this process occurs every 3 to 4 days. The rapid turnover of skin cells results in the accumulation of dead skin cells on the surface, causing the characteristic scaly patches.
Genetics: People having a family history of psoriasis are more likely to develop the condition, although environmental factors, infections, and lifestyle choices can also trigger its onset or exacerbate symptoms.
Common Triggers of Psoriasis
While psoriasis is an autoimmune disorder, certain factors can trigger or worsen symptoms:
- Infections: Infections, whether bacterial or viral, such as strep throat, can trigger flare-ups of psoriasis, particularly in cases of guttate psoriasis.
- Stress: Psoriasis is known to worsen in response to emotional stress because it can influence the immune system’s response.
- Weather: While sunshine and humid temperatures frequently relieve psoriasis symptoms, cold, dry weather can worsen symptoms by drying the skin.
- Injury to the Skin: Cuts, scrapes, or severe sunburns can lead to a psoriasis flare in a phenomenon known as the Koebner response.
- Medications: Certain medications, such as lithium, beta-blockers, and antimalarial drugs, have been linked to the onset or worsening of psoriasis.
- Alcohol and Smoking: Both smoking and excessive alcohol consumption can aggravate psoriasis and reduce the effectiveness of treatment.
Psoriatic Arthritis
In some cases, psoriasis can lead to a form of arthritis known as psoriatic arthritis, which causes joint pain, stiffness, and swelling. Psoriatic arthritis can develop gradually or suddenly and can affect any joint in the body. It is a serious condition that, if left untreated, can lead to permanent joint damage.
Diagnosis and Treatment
Psoriasis is typically diagnosed through a physical examination of the skin, although a biopsy may be conducted to rule out other conditions. There is no cure for psoriasis, but various treatment options can help manage symptoms and improve quality of life.
Treatment Options
- Topical Treatments: For mild to moderate psoriasis, creams and ointments are often prescribed to reduce inflammation, slow the production of skin cells, and soothe itching. Common topical treatments include corticosteroids, vitamin D analogues, and salicylic acid.
- Phototherapy: Also known as light therapy, this treatment involves exposing the skin to ultraviolet (UV) light under medical supervision. Phototherapy slows down skin cell turnover and reduces inflammation. Both UVB and UVA treatments are used, depending on the severity of the condition.
- Systemic Medications: For more severe cases of psoriasis, oral or injected medications may be prescribed to suppress the immune system. These include methotrexate, cyclosporine, and biologics (targeted therapies that block specific proteins involved in the immune response).
- Lifestyle Modifications: In addition to medical treatments, lifestyle changes can help manage symptoms. Keeping the skin moisturized, avoiding known triggers (such as stress and smoking), and adopting a healthy diet rich in anti-inflammatory foods can support better skin health and reduce flare-ups.
- Biologics: A newer class of drugs, biologics are often used to treat moderate to severe psoriasis. These medications target specific parts of the immune system, such as tumour necrosis factor-alpha (TNF-alpha) or interleukins, which are involved in the inflammation process.
- Alternative Therapies: Some individuals seek relief from psoriasis through alternative treatments, such as acupuncture, yoga, or supplements like fish oil. While these approaches may not be a cure, they can complement traditional treatments and improve overall well-being.
Conclusion
While psoriasis is a chronic condition with no cure, it can be managed effectively with the right combination of medical treatments, lifestyle modifications, and support. Understanding the triggers, symptoms, and treatment options is key to controlling flare-ups and improving the quality of life for those affected by psoriasis. If you or a loved one is experiencing symptoms of psoriasis, consult a healthcare professional for an accurate diagnosis and personalized treatment plan.