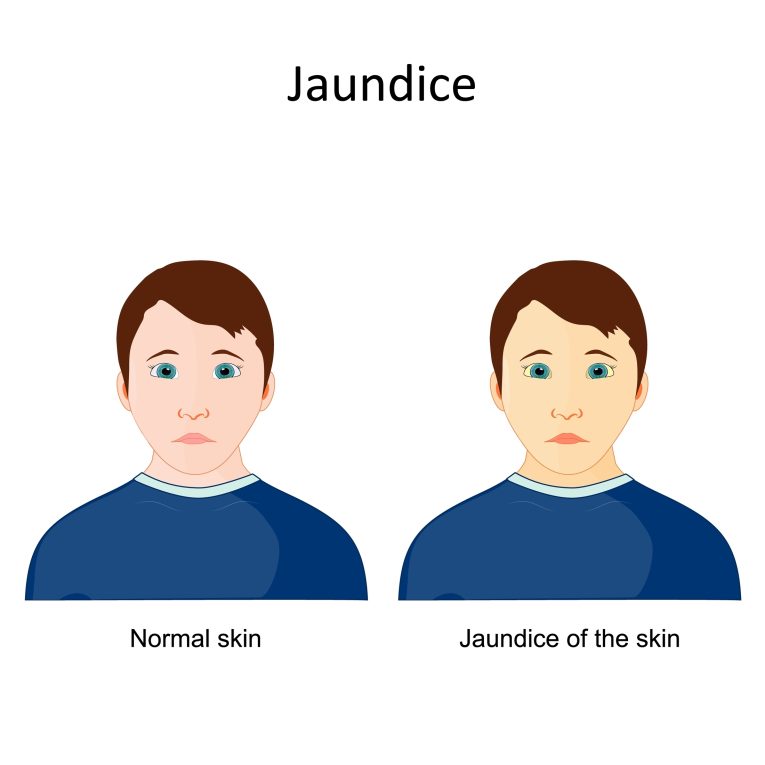
Jaundice, or icterus is a condition that is often recognized by the yellowing of the skin and eyes, caused by an increase in the levels of bilirubin in the blood. Although jaundice is often associated with newborns, it can affect people of all ages. This blog will provide a comprehensive overview of jaundice, its causes, symptoms, treatment, and preventive measures.
What is Jaundice?
Jaundice itself is not a disease but a symptom of an underlying condition that affects the liver, red blood cells, or bile ducts. Bilirubin is a yellow pigment formed by the breakdown of red blood cells in the body. The liver is responsible for filtering out bilirubin from the blood and excreting it through the bile. When there is a disruption in this process, bilirubin accumulates, causing the characteristic yellow discolouration of the skin, eyes, and mucous membranes.
Types of Jaundice:
Icterus/jaundice is classified into three main types based on where the disruption occurs:
- Pre-hepatic Jaundice (Hemolytic Jaundice): This type occurs due to an increase in the breakdown of red blood cells, leading to excessive bilirubin production that the liver cannot process efficiently. Conditions such as hemolytic anaemia, sickle cell anaemia, and malaria can cause pre-hepatic jaundice.
- Hepatic Jaundice: Hepatic jaundice results from liver dysfunction. When the liver is unable to process and excrete bilirubin effectively due to conditions like hepatitis, liver cirrhosis, or liver cancer, bilirubin builds up in the blood. Alcohol-related liver damage is also a common cause of hepatic jaundice.
- Post-hepatic Jaundice (Obstructive Jaundice): This type of jaundice is caused by a blockage in the bile ducts, preventing bilirubin from being excreted through bile. Gallstones, tumours, or strictures in the bile ducts can result in post-hepatic jaundice.
Causes of Jaundice:
Why jaundice occur? It’s a frequently asked question that many people are curious about; the causes of jaundice can vary depending on the underlying condition. Some of the most common causes include:
- Liver Diseases: Conditions like hepatitis (both viral and autoimmune), cirrhosis, and liver cancer are common causes of jaundice. These diseases impair the liver’s ability to filter and excrete bilirubin properly.
- Hemolytic Anaemia: In conditions like hemolytic anaemia, the rapid breakdown of red blood cells leads to an excessive release of bilirubin, overwhelming the liver’s capacity to excrete it.
- Gallstones: Gallstones can block the bile ducts, preventing bile (and the bilirubin it carries) from being excreted. This leads to a buildup of bilirubin in the blood, resulting in jaundice.
- Pancreatic Cancer: Tumours in the pancreas can obstruct the bile ducts, leading to post-hepatic jaundice.
- Genetic Disorders: Some inherited conditions, like Gilbert’s syndrome, can result in mild jaundice due to reduced ability of the liver to process bilirubin.
- Newborn Jaundice: Jaundice in newborns is common due to the immaturity of their liver, which may not yet efficiently process bilirubin. This usually resolves on its own within a few days to weeks.
Symptoms of Jaundice:
The most common symptom of jaundice is the yellowing of the skin and the whites of the eyes. However, other symptoms can accompany this, depending on the underlying cause. These include:
- Dark urine: Bilirubin can make urine darker than usual, often described as tea-coloured or brown.
- Pale stools: If bilirubin cannot enter the intestines, the stool may appear lighter in colour, sometimes almost white or clay-like.
- Itching (Pruritus): The buildup of bile salts in the skin can lead to intense itching.
- Fatigue: Chronic liver diseases can result in extreme tiredness or weakness.
- Abdominal pain: Conditions like gallstones or liver inflammation may cause pain in the upper right side of the abdomen.
- Nausea and vomiting: These symptoms often accompany liver-related causes of jaundice.
- Weight loss: Unintentional weight loss can occur in cases of liver disease or cancer.
Diagnosis of Jaundice:
To diagnose jaundice and its underlying cause, a doctor will typically conduct a thorough medical history, physical examination, and diagnostic tests. The following tests may be used:
- Blood tests: These include liver function tests (LFTs) to check the levels of bilirubin and other liver enzymes. A complete blood count (CBC) can also assess hemolysis.
- Ultrasound: This imaging technique is used to examine the liver, gallbladder, and bile ducts for any abnormalities or blockages.
- CT Scan or MRI: These advanced imaging techniques provide detailed views of the liver, pancreas, and bile ducts, helping to identify tumours or other obstructions.
- Liver biopsy: A small sample of liver tissue may be taken to determine the cause of liver disease, especially in cases of suspected liver cancer or cirrhosis.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure is used to examine the bile ducts and pancreas for blockages.
Treatment of Jaundice:
The treatment of jaundice depends on the underlying cause. There is no direct treatment for icterus itself, but managing the root cause can alleviate the symptoms.
- Jaundice Medicine:
- For Hepatitis: Antiviral or corticosteroid medications may be prescribed for viral or autoimmune hepatitis.
- For Hemolytic Anaemia, Treatment includes managing the underlying cause of red blood cell destruction, such as blood transfusions or medications that suppress the immune system.
- For Infections: Antibiotics may be needed if the jaundice is caused by an infection.
- Surgical Intervention:
- Gallstones: If gallstones are blocking the bile ducts, surgery may be required to remove them.
- Cancer: Surgery, chemotherapy, or radiation may be necessary to treat tumours that are obstructing the bile ducts.
- Phototherapy:
- In newborns, phototherapy (light therapy) is commonly used to treat icterus by breaking down bilirubin in the skin.
- Lifestyle Changes:
- In cases of alcohol-induced liver disease, abstaining from alcohol is crucial for liver recovery. A healthy diet low in fats and rich in fruits, vegetables, and whole grains can also support liver function.
Prevention of Jaundice
Preventing jaundice involves addressing the conditions that cause it. Here are some steps that can help:
- Vaccination: Getting vaccinated for hepatitis A and B can prevent liver infections that lead to jaundice.
- Safe Alcohol Consumption: Limiting alcohol intake can prevent liver damage, such as cirrhosis.
- Maintain a Healthy Weight: Obesity is linked to fatty liver disease, which can lead to jaundice.
- Practice Safe Hygiene: Hepatitis A is transmitted through contaminated food and water, so practising good hygiene and eating clean, cooked food can prevent infection.
- Avoid Illicit Drugs: Using drugs that can harm the liver or sharing needles can lead to liver damage and jaundice.
Summary of Jaundice:
Jaundice is a visible sign that something is wrong with the body’s bilirubin processing, often related to liver or blood disorders. While it can range from mild to severe, early diagnosis and treatment of the underlying cause are essential to prevent complications. Maintaining liver health through a balanced diet, safe alcohol consumption, and timely medical care is key to preventing conditions that can lead to jaundice.