Liver cirrhosis is a serious and potentially life-threatening condition that occurs when healthy liver tissue is replaced with scar tissue, leading to long-term damage and impaired liver function. The liver plays a critical role in digestion, detoxification, and metabolic processes, so any disruption can significantly impact overall health.
What Is Liver Cirrhosis?
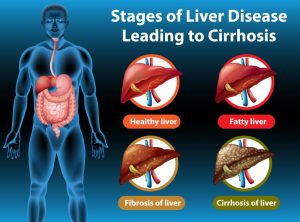
Cirrhosis is the final stage of chronic liver disease. Over time, continuous injury to the liver—due to alcohol, infection, fat buildup, or toxins—leads to fibrosis, or scarring. In cirrhosis, this scarring becomes so extensive that it disrupts the structure and function of the liver.
Cirrhosis is irreversible, but early detection and management can slow its progression and prevent life-threatening complications.
Pathogenesis of Liver Cirrhosis
Pathogenesis of liver cirrhosis refers to the sequence of events and mechanisms that lead to the development of cirrhosis, the end stage of chronic liver disease. Here’s a concise breakdown:
1. Ongoing Liver Damage
The liver gets damaged again and again — usually from:
-
Too much alcohol
-
Hepatitis B or C infections
-
Fat building up in the liver (fatty liver disease)
-
Problems with the immune system or bile ducts
2. Inflammation Starts
The damaged liver cells send out signals asking for help.
This causes the body to send immune cells to the liver, which causes inflammation (swelling and irritation).
3. Scar Tissue Formation
Special cells in the liver (called stellate cells) get activated.
They start producing scar tissue to repair the damage — like a bandage.
4. Too Much Scar Tissue
Over time, too much scar tissue builds up.
This blocks blood flow and messes up the liver’s structure.
Healthy liver tissue gets replaced by fibrous (scarred) areas.
5. Liver Becomes Hard and Lumpy
Because of repeated damage and scarring:
-
The liver becomes hard instead of soft
-
It forms lumps (nodules) as it tries to grow new cells
6. Blood Flow Problem
The scarring blocks blood flow through the liver → causing high pressure in the veins (called portal hypertension).
This leads to problems like swollen belly (ascites), bleeding, and confusion.
7. Liver Can’t Work Properly
As more liver tissue gets damaged:
-
The liver stops doing its job — like removing toxins or making important proteins.
-
This is called liver failure
Causes of Liver Cirrhosis
Many factors can cause liver damage that progresses to cirrhosis. Some of the most common include:
1. Chronic Alcohol Abuse
Heavy and prolonged alcohol consumption is a major cause of cirrhosis. Alcohol damages liver cells, leading to inflammation and scarring over time.
2. Viral Hepatitis
- Hepatitis B and C are viral infections that can lead to chronic liver inflammation and, eventually, cirrhosis.
- Hepatitis C is a leading cause of liver transplants worldwide due to cirrhosis and liver cancer risk.
3. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is increasingly common due to rising obesity, diabetes, and metabolic syndrome. When fat builds up in the liver, leading to inflammation and damage, it’s called Non-Alcoholic Steatohepatitis (NASH), which can progress to cirrhosis.
4. Autoimmune Hepatitis
This is a condition where the immune system mistakenly attacks liver cells, causing chronic inflammation and scarring.
5. Inherited Liver Diseases
Certain genetic conditions like:
- Hemochromatosis (iron overload)
- Wilson’s disease (copper accumulation) can lead to cirrhosis if untreated.
6. Bile Duct Diseases
Conditions like Primary Biliary Cholangitis (PBC) or Primary Sclerosing Cholangitis (PSC) involve damage to bile ducts, leading to bile buildup and liver injury.

Symptoms of Liver Cirrhosis
Cirrhosis may remain asymptomatic in its early stages. As it progresses, signs and symptoms begin to appear, including:
- Fatigue and weakness
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Jaundice (yellowing of the skin and eyes)
- Swelling in legs, feet, or abdomen (ascites)
- Easy bruising or bleeding
- Itchy skin
- Spider-like blood vessels on the skin
- Confusion or memory problems (hepatic encephalopathy)

Stages of Cirrhosis
Cirrhosis is classified into compensated and decompensated stages:
1. Compensated Cirrhosis
- Liver is scarred but still functions relatively well.
- Patients may not experience significant symptoms.
- Early detection is critical in this stage.
2. Decompensated Cirrhosis
- Liver function is significantly impaired.
- Symptoms like ascites, jaundice, variceal bleeding, and encephalopathy appear.
- This stage requires intensive medical care and may lead to liver failure.
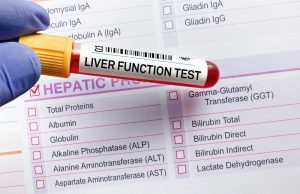
How Is Liver Cirrhosis Diagnosed?
The liver cirrhosis tests are as follows:
1. Blood Tests
- Liver function tests (ALT, AST, bilirubin, albumin)
- Coagulation profile (INR)
- Viral markers (Hepatitis B & C)
- Autoimmune and metabolic panels
2. Imaging Tests
- Ultrasound helps assess liver size, texture, and presence of ascites.
- FibroScan (Transient Elastography) measures liver stiffness.
- CT or MRI may help visualize complications like tumors or portal hypertension.
3. Liver Biopsy
- In select cases, a biopsy may be done to confirm cirrhosis and evaluate its cause.
Complications of Liver Cirrhosis
If untreated, cirrhosis can lead to several serious complications:
1. Portal Hypertension
Scarring blocks blood flow through the liver, increasing pressure in the portal vein, leading to:
- Esophageal and gastric varices (which may rupture and bleed)
- Splenomegaly (enlarged spleen)
- Ascites
2. Ascites
Fluid accumulation in the abdominal cavity. Increases the risk of spontaneous bacterial peritonitis (SBP).
3. Hepatic Encephalopathy
The liver can no longer filter toxins like ammonia, which affects brain function—causing confusion, altered behavior, and in severe cases, coma.
4. Liver Cancer (Hepatocellular Carcinoma)
Cirrhosis is the main risk factor for liver cancer, especially in hepatitis B/C and alcohol-related liver disease.
5. Kidney Dysfunction (Hepatorenal Syndrome)
Advanced cirrhosis can lead to progressive kidney failure.

Treatment of Liver Cirrhosis
While cirrhosis cannot be reversed, its progression can be slowed, and complications managed through:
1. Treating the Underlying Cause
- Stop alcohol use completely.
- Antiviral therapy for hepatitis B/C.
- Weight loss and diabetes control for NAFLD.
- Chelation therapy for iron/copper overload in hereditary diseases.
2. Managing Complications
- Diuretics and low-sodium diet for ascites.
- Endoscopic banding or beta-blockers for variceal bleeding prevention.
- Lactulose and rifaximin for hepatic encephalopathy.
- Paracentesis for draining ascitic fluid.
- Monitoring for liver cancer with periodic ultrasound and AFP blood tests.
3. Liver Transplantation
For patients with decompensated cirrhosis or liver failure, liver transplant is the only curative option. Patient selection is based on MELD score (Model for End-Stage Liver Disease) and overall health condition.
Liver Cirrhosis Care Plan
✅ Healthy Diet
- High-protein (unless encephalopathy is present)
- Low-sodium to prevent fluid retention
- Avoid raw seafood (to prevent infections)
- Avoid herbal or over-the-counter medications unless prescribed
✅ Avoid Alcohol and Smoking
Complete abstinence is mandatory, even if alcohol was not the original cause.
✅ Vaccinations
Patients should receive Hepatitis A, B, influenza, and pneumococcal vaccines to prevent infections.
✅ Regular Monitoring
- Liver function tests every few months
- Endoscopy to check for varices
- Cancer screening every 6 months
Can Cirrhosis of the Liver Be Reversed?
-
Early stage (fibrosis): Yes, it can be reversed if the cause is treated early.
-
Late stage (cirrhosis): Usually not fully reversible, but progression can be slowed or stopped.
What helps?
-
Stop alcohol
-
Treat hepatitis
-
Regular check-ups
In severe cases, a liver transplant may be needed.
Living with Cirrhosis: Emotional and Practical Support
Cirrhosis affects every part of a patient’s life. Fatigue, dietary restrictions, frequent hospital visits, and emotional stress can be overwhelming. Support from family, counseling, and patient education can help improve quality of life.
Joining a liver support group, either in person or online, helps patients feel less alone in their journey and offers shared experiences and coping strategies.
Conclusion:
Liver cirrhosis is a progressive and chronic liver disease with serious consequences if left untreated. However, with early diagnosis, lifestyle changes, medical management, and regular follow-up, many patients can live longer, healthier lives.
At Omega Hospitals, we offer comprehensive liver care, including early diagnosis, treatment of underlying causes, management of complications, and liver transplant support. Our multidisciplinary team of hepatologists, gastroenterologists, dietitians, and liver transplant surgeons ensures that every patient receives personalized, evidence-based care.
FAQ’s
- Which doctor treats liver disease?
A gastroenterologist or a hepatologist usually treats liver diseases.
2. Can liver cirrhosis be present without symptoms?
Yes. In early stages, cirrhosis may have no symptoms. It’s often discovered through routine tests or during evaluation for another condition.
3. Can someone live a long life with liver cirrhosis?
Yes — especially if diagnosed early and the underlying cause is treated. Many patients live for years with lifestyle changes and proper medical care.
4. Is cirrhosis only caused by alcohol?
No. Other causes include hepatitis B & C, fatty liver disease, autoimmune diseases, and genetic conditions like Wilson’s disease.
5. Can the liver regenerate after cirrhosis?
The liver has the ability to regenerate, but in advanced cirrhosis, the scarring limits this. Early treatment can improve regeneration chances.
6. Is liver cirrhosis contagious?
No, cirrhosis itself is not contagious. But hepatitis B and C, which can lead to cirrhosis, are contagious through blood or bodily fluids.
7. Does liver cirrhosis always need a transplant?
No. Only end-stage or decompensated cirrhosis may need a transplant. Many people manage well with medications and lifestyle changes.
8. Can liver cirrhosis affect mental health?
Yes. Cirrhosis can lead to hepatic encephalopathy, a condition where toxins affect brain function, causing confusion, memory issues, or behavior changes.
9. Is cirrhosis reversible if you stop drinking?
If caught early, stopping alcohol can halt or slightly reverse the damage. But advanced cirrhosis may not reverse, though stopping alcohol is still vital.
10. Can cirrhosis patients eat everything?
No. They need a liver-friendly diet – low in salt, balanced in protein, and no alcohol. Raw seafood and processed foods should be avoided.

