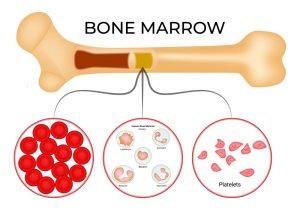
Blood cancer is one of the most critical health challenges today, affecting millions worldwide. It starts in the blood-forming tissues, such as the bone marrow or the lymphatic system, and impacts the body’s ability to produce and functionally utilize blood cells. The three major types of blood cancer—leukaemia, lymphoma, and multiple myeloma—can affect people of all ages.
Understanding the factors that cause blood cancer is essential for early diagnosis, prevention, and effective treatment. While the exact cause of blood cancer is often unknown, several risk factors have been identified through decades of research.
1. Genetic Mutations and Family History
One of the most well-documented factors in the development of blood cancer is genetic mutation. Changes in DNA within blood-forming cells can lead to abnormal cell division and survival. These mutations can occur spontaneously or be inherited.
- Inherited genetic syndromes such as Li-Fraumeni syndrome, Down syndrome, and Fanconi anaemia can increase susceptibility.
- If a close family member (especially a parent or sibling) has had leukaemia or lymphoma, the risk may be slightly higher.
- Though most blood cancers are not directly inherited, a family history can indicate a shared genetic or environmental risk.

2. Exposure to Radiation
Exposure to high levels of ionizing radiation is a known risk factor for blood cancer, particularly leukaemia.
- Atomic bomb survivors, nuclear plant workers, and those who have undergone radiation therapy for other cancers are at higher risk.
- Diagnostic radiation (like X-rays or CT scans) poses a minimal risk, but cumulative exposure over time could add up.

3. Chemical Exposure
Long-term exposure to certain chemicals can damage the bone marrow, leading to the development of blood cancers.
- Benzene, a widely used industrial chemical found in paints, plastics, and cigarette smoke, is a known carcinogen.
- Formaldehyde, used in building materials and household products, has also been linked to leukaemia.
- People working in the rubber industry, oil refineries, or chemical plants are often at higher risk due to consistent chemical exposure.

4. Weakened Immune System
The immune system plays a crucial role in identifying and destroying abnormal cells. A weakened or suppressed immune system can make the body more vulnerable to blood cancers.
- People with autoimmune disorders like lupus or rheumatoid arthritis may have a slightly increased risk.
- Organ transplant recipients, who take immunosuppressant medications, are also more susceptible.
- Those with HIV/AIDS face higher rates of certain blood cancers, particularly non-Hodgkin lymphoma.

5. Viral Infections
Certain viruses have been associated with the onset of blood cancers by directly altering DNA in blood cells or weakening the immune system.
- Epstein-Barr Virus (EBV) – linked to Burkitt lymphoma and Hodgkin lymphoma.
- Human T-cell leukaemia virus type 1 (HTLV-1) – associated with adult T-cell leukaemia/lymphoma.
- Hepatitis C virus (HCV) – increases the risk of developing non-Hodgkin lymphoma.
- Human herpesvirus 8 (HHV-8) – associated with Kaposi’s sarcoma and primary effusion lymphoma.

6. Age and Gender
Age is a non-modifiable but significant risk factor.
- Leukaemia is most common in children and older adults, while multiple myeloma and non-Hodgkin lymphoma typically affect people over 60.
- Certain types of blood cancer are more common in men than women, although the reasons are still not entirely clear. Hormonal, lifestyle and genetic factors may play a role.

7. Smoking and Tobacco Use
Smoking doesn’t just harm the lungs—it has systemic effects.
- Tobacco smoke contains benzene and other carcinogens that can damage bone marrow and lead to leukemia, especially acute myeloid leukemia (AML).
- Even secondhand smoke exposure can contribute to increased cancer risk, particularly in children.

8. Obesity and Poor Lifestyle Habits
Emerging evidence shows that lifestyle choices can influence the risk of blood cancer.
- Obesity increases inflammation in the body, alters hormone levels, and can suppress immune function—all of which can contribute to cancer development.
- Lack of physical activity and poor nutrition also increase the overall risk of several cancers, including lymphoma.

9. Previous Cancer Treatment
Ironically, certain treatments used to cure cancers can also increase the risk of developing blood cancer later.
- Chemotherapy drugs, especially alkylating agents, have been associated with secondary leukaemia.
- Radiation therapy to treat other types of cancers may damage healthy bone marrow cells, particularly in children and young adults.

10. Environmental and Occupational Hazards
Long-term exposure to pollutants and hazardous work conditions increases the likelihood of blood cancer.
- Agricultural workers exposed to pesticides and herbicides may face increased risk.
- Industrial jobs involving solvents, heavy metals, or gasoline can also pose a threat.
- Even prolonged exposure to indoor pollutants like formaldehyde in poorly ventilated spaces could contribute.

11. Chronic Inflammation and Bone Marrow Disorders
Conditions that cause chronic inflammation or ongoing stress to the bone marrow may lead to blood cancers over time.
- Myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPNs) are bone marrow disorders that can evolve into leukaemia.
- Persistent inflammation may lead to DNA damage and promote cancer cell growth.
12. Geographic and Socioeconomic Factors
Where you live and your access to healthcare can affect both exposure and early detection.
- People living in industrialized or heavily polluted areas might have a higher exposure to carcinogens.
- Those from low socioeconomic backgrounds often face delays in diagnosis, poor access to healthcare, and are more exposed to environmental toxins.

Final Thoughts: Can Blood Cancer Be Prevented?
While many blood cancer causes are beyond personal control—like age, genetics, or unavoidable radiation exposure—there are several preventive steps individuals can take:
- Avoid smoking and exposure to secondhand smoke.
- Maintain a healthy weight and stay physically active.
- Use protective gear if you work around chemicals or in high-risk environments.
- Get regular checkups, especially if you have a family history of cancer.
- Manage chronic infections and immune conditions under medical supervision.
Conclusion:
Blood cancer is a complex disease influenced by a combination of genetic, environmental, viral, and lifestyle factors. While not all causes are preventable, increased awareness and proactive health measures can significantly reduce risk and improve outcomes.
Early detection and access to advanced treatment have transformed survival rates in recent years. If you or someone you know experiences unexplained fatigue, frequent infections, bruising, or swollen lymph nodes, don’t ignore the signs—seek medical attention promptly.
By understanding these risk factors, we empower ourselves to make better choices, encourage early diagnosis, and potentially save lives.